In the not-too-distant future, a revolutionary new type of immunotherapy – CAR NKT therapy – is expected to be available for the treatment of pediatric neuroblastoma and potentially other types of solid-tumor cancers.
In this immunotherapy, a chimeric antigen receptor (CAR) is used to genetically modify natural killer T-cells (NKTs) to target solid tumors.
For patients with neuroblastoma, 90 percent of whom are children under the age of 5, this means the potential to replace harsh chemotherapy and radiation therapy with much less toxic, more targeted and shorter treatment. At a minimum, the goal is to have a viable option for use alongside chemotherapy and radiation to eliminate the cancers that resist traditional treatment or have relapsed.
Neuroblastoma tumors form in nerve tissue, often starting in the adrenal glands and spreading to the chest, spine and abdomen. Because the tumors can grow very large very quickly, it is difficult to treat surgically unless it is caught very early, which is not typically the case. The long-term survival rate of high-risk and refractory neuroblastoma in the US is only 45 percent, with an overall US survival rate of approximately 80 percent.
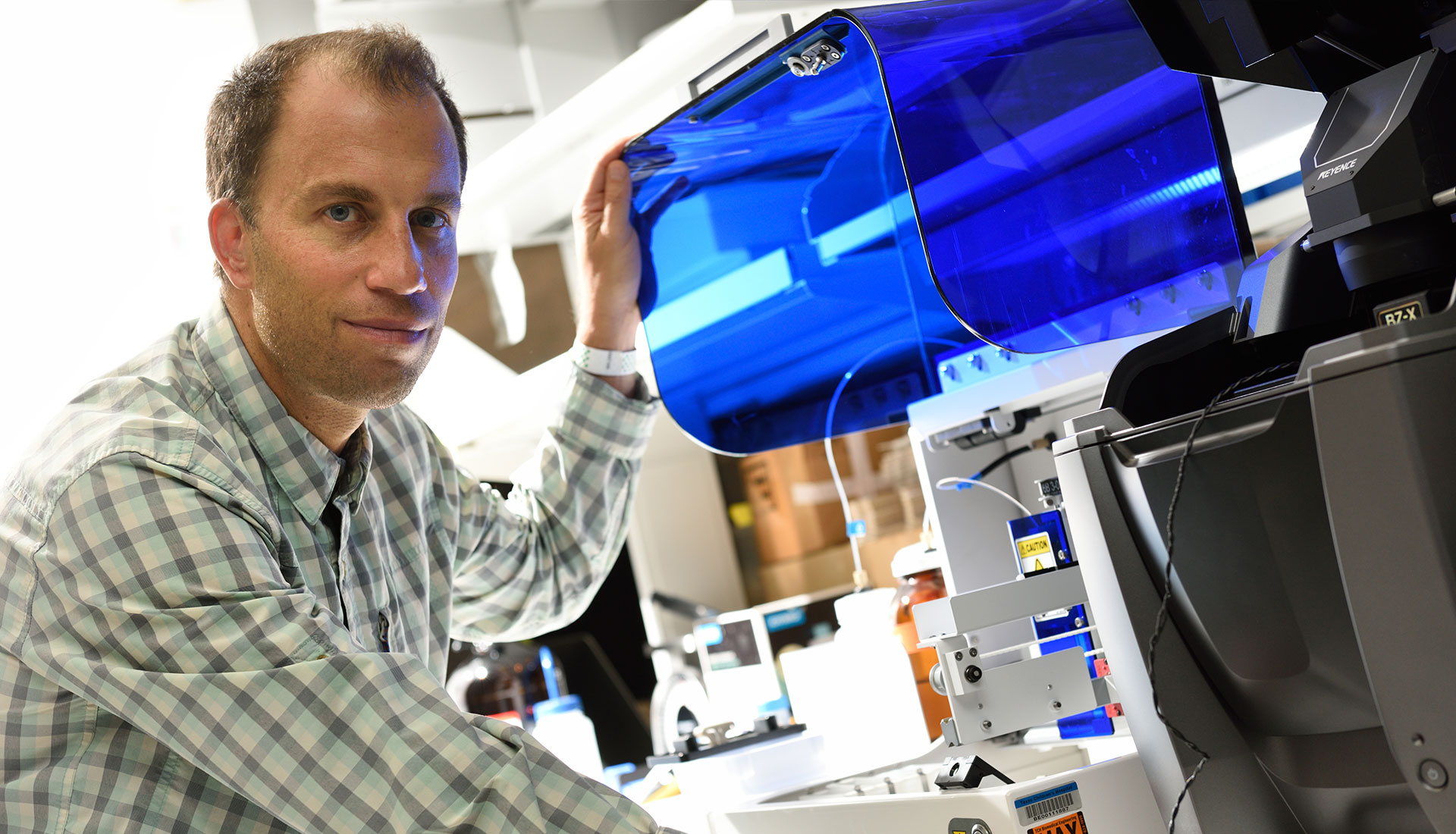
The drive to cure 100 percent of neuroblastoma patients and the incredible promise of CAR NKT therapy are what motivate physician-scientists Leonid Metelitsa, MD, PhD, co-director of the Neuroblastoma Program at Texas Children’s Hospital and professor in the Department of Pediatrics, Section of Hematology-Oncology at Baylor College of Medicine, and Andras Heczey, MD, director of the Liver Tumor Program at Texas Children’s and assistant professor in the Department of Pediatrics, Section of Hematology-Oncology at Baylor.
For more than a decade, Metelitsa and Heczey have studied immune cells to identify a way to eradicate solid tumors using immunotherapy – an achievement that has, to date, largely eluded the medical community.
“For neuroblastoma cases that are more difficult to treat, little progress has been made in the last 30 years,” Metelitsa said. “With immunotherapy, in general, solid tumors have posed a challenge. Other forms of immunotherapy have been successful in treating certain types of cancers, including melanoma, lung cancer and some blood cancers, such as leukemia and lymphoma, but not yet in children with neuroblastoma.”
It is hoped that this is about to change.
What started as a research breakthrough in 2009 has been tested and is now in the midst of a phase 1 clinical trial by Baylor and Texas Children’s. It is the first clinical trial in the world examining the effectiveness of CAR and NKTs combined into one treatment in humans.
CAR NKT therapy leverages the natural ability of the immune system to fight cancer in a way that chemotherapy and radiation cannot. It trains the body’s own natural killer T-cells (NKTs) to recognize and destroy cancer tumors with an extra boost from synthetic additives.
A vital part of the immune system, NKTs are especially effective at destroying cancer tumors. NKTs have properties that enable them to attack specialized cells inside solid tumors that encourage tumor growth and inhibit the immune system response. Even on their own, without any genetic modification, the deployment of NKTs in the treatment of neuroblastoma and other types of cancer tumors is associated with better outcomes.
However, the low frequency of NKTs in human blood cells – less than 0.1 percent and even lower in cancer patients – necessitated the development of novel methods for increasing their number for cancer treatment. Over the last 15 years, prior clinical trials conducted by researchers in the US and Japan using cancer-patient-derived NKTs suffered from low and highly variable frequencies of NKTs in the treatments – ranging from 2 to 90 percent.
Protocols developed in the labs at Texas Children’s Cancer Center enabled a large-scale expansion of NKTs from both healthy individuals and cancer patients with 90 to 99 percent purity.
The work was pioneered on-site in labs at Texas Children’s Cancer Center and the Center for Cell and Gene Therapy (CAGT), where Metelitsa and Heczey are members. Physicians across departments at Baylor and Texas Children’s work collaboratively at CAGT – led by Helen Heslop, MD – to share knowledge and further develop new immunotherapy treatments.
“It’s pretty unique that a product such as CAR NKT therapy is being manufactured in-house and that we have such robust collaboration across the institution. The Center for Cell and Gene Therapy is one of the largest centers of this type in the US,” Metelitsa said.
The Baylor-Texas Children’s protocol for CAR NKT therapy consists of multiple steps with the objective to suppress tumor growth and eventually make tumors disappear:
 (Left) Andras Heczey, MD, looks forward to cancer treatments without the toxic side effects of chemotherapy and radiation.
(Left) Andras Heczey, MD, looks forward to cancer treatments without the toxic side effects of chemotherapy and radiation.The clinical trial, known as GINAKIT2, began in the fall of 2018 and continues today.
During phase 1 of the clinical trial, which encompasses the initial administration of CAR NKT therapy, Metelitsa and Heczey seek to:
Patients under the age of 18 with high-risk neuroblastoma (refractory or recurrent cases) volunteer to travel to Houston for treatment from across the US. All participants undergo CAR NKT therapy as part of the study.
The first three patients received a very low initial dose of NKTs, and subsequent patients receive higher doses. The infusion is followed by a four-week monitoring period, after which the patient and his or her family may either stop treatment or opt for additional treatment. Metelitsa and Heczey hope to enroll up to 24 patients.
So far, the results have been very promising. Of the three original patients, two achieved a stable disease with no progression in tumor growth. One patient experienced a near complete regression of the neuroblastoma tumor and remained progression free for more than three months.
Side effects specific to CAR NKT therapy are not yet well understood, but none of the first three patients suffered any significant negative side effects.
“I’m very excited by these results, which show significant anti-tumor activity even with a low dose of NKTs. There is tremendous potential in this therapy,” Heczey said. “I look forward to monitoring the progress of these patients and increasing the dosage of CAR NKTs.”
But there’s still a long road ahead.
“The number of pediatric neuroblastoma patients who fit the study criteria is low compared to the number of other solid tumors in adults. We have to accumulate enough patients to move through the second and third phases of the clinical trial. The most optimistic scenario for getting a widely available CAR NKT therapy to market is five to six years,” Metelitsa said.
One of the most exciting aspects of this clinical trial is its broader applicability to other types of pediatric cancers comprising solid tumors. In fact, it’s already happening with the two most common types of pediatric liver cancer: hepatoblastoma and hepatocellular carcinoma (HCC). These two types of liver cancer alone account for about 95 percent of all pediatric liver cancers.
Currently, HCC has a long-term survival rate of only 20 percent. For hepatoblastoma, it’s about 80 percent, but treatment for both types involves long, intensive rounds of chemotherapy.
Heczey oversees a clinical trial, known as GAP, which began in August 2019 for treating these liver cancers using CAR T therapy. CAR T therapy works similarly to CAR NKT therapy, but without the enhanced abilities of NKTs. Instead, CAR is combined with regular T-cells. In this treatment, CAR helps T-cells target Glypican-3, the molecule expressed on the surface of liver tumors.
In addition, Heczey already has begun exploring the use of NKTs to treat these liver cancers.
“With CAR NKT therapy, I hope to establish that we can increase therapeutic potency while avoiding damage to the rest of the body from prolonged exposure to chemicals and preventing secondary malignancy associated with more toxic chemotherapy and radiation. Perhaps one day this type of immunotherapy can become a primary, front-and-center form of treatment that is successful on its own. This would be a great achievement for patients,” Heczey said.