Remember Goldilocks trying to find the porridge, chair and bed that were “just right”?
Scientists acknowledge that a Goldilocks effect seems to exist in areas as diverse as astronomy, psychology and microbiology. Too little and too much both cause problems.
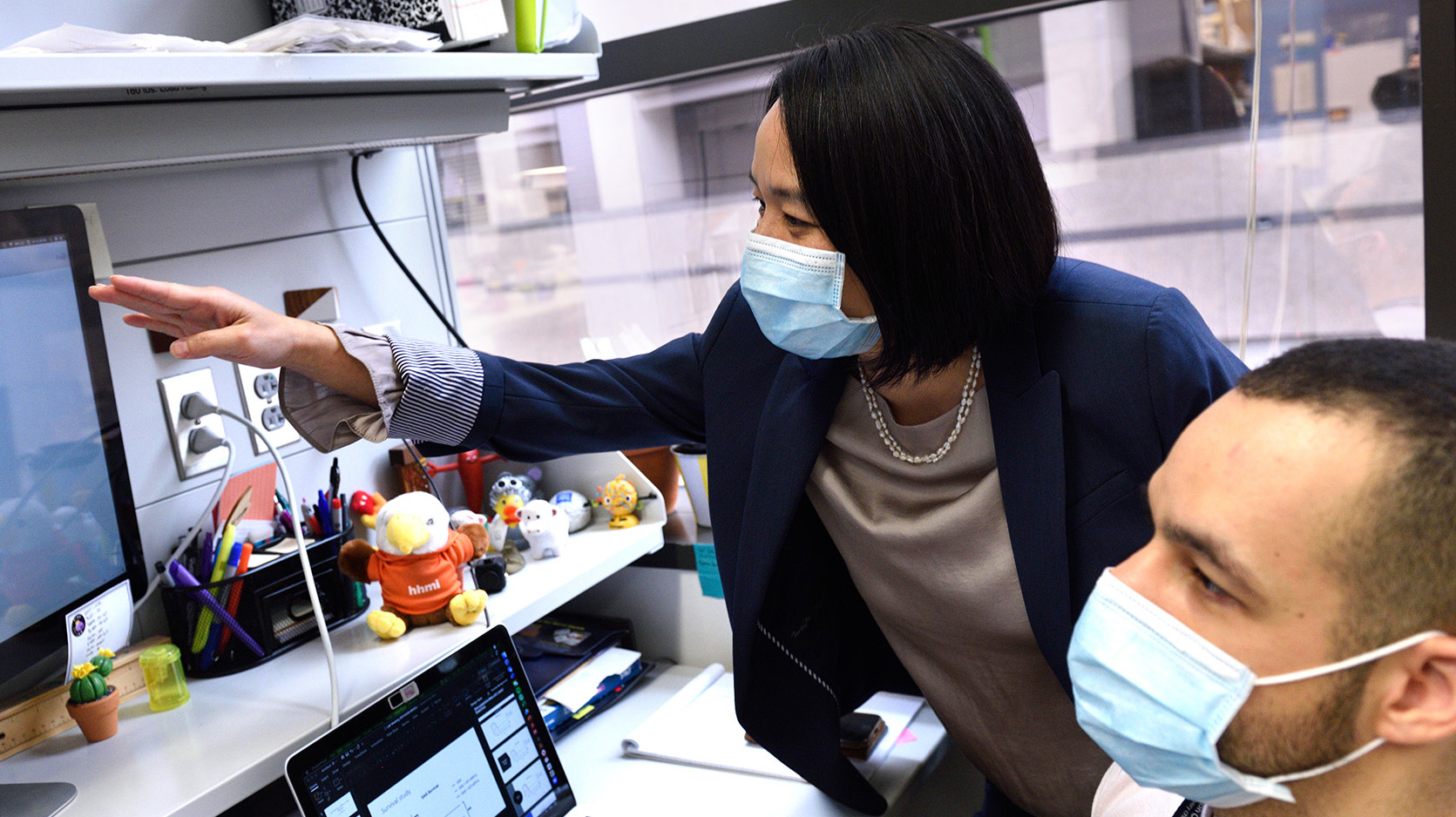
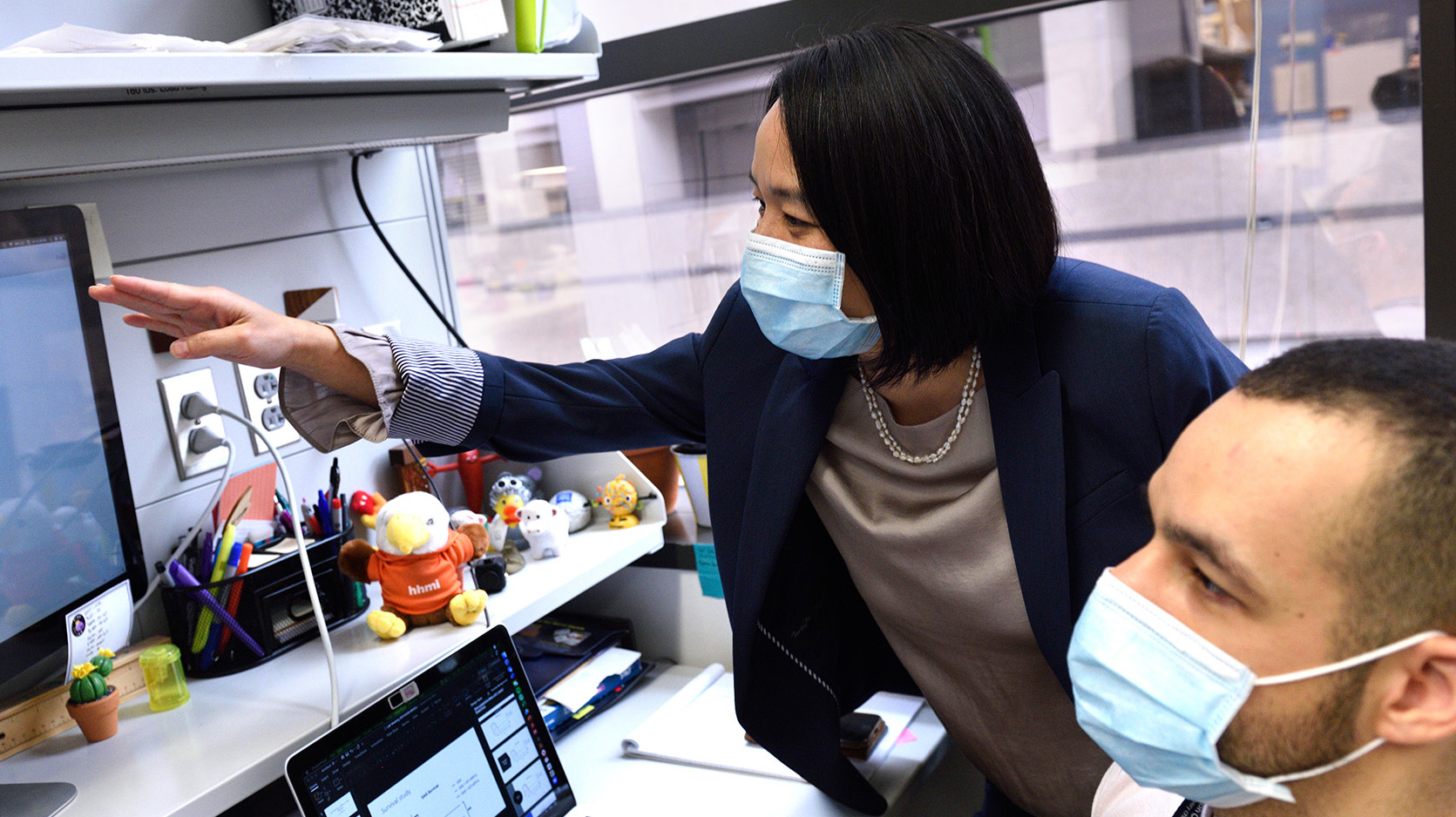
Katherine Y. King, MD, PhD, leads research into effects of inflammation on blood production by stem cells in the bone marrow. Dr. King is associate vice chair for research and associate professor of pediatrics-infectious disease in the Department of Pediatrics at Baylor College of Medicine and Texas Children’s Hospital.
“You can’t have too much, and you can’t have too little,” she said about inflammation.
When a person has an infection, inflammatory signals tell stem cells in the bone marrow to produce more immune cells in the blood to fight the infection. If there are too few signals, the infection goes unchecked. But too many inflammatory signals, such as from infection or another stress, can lead to depletion of the stem cells in the bone marrow. That could cause bone marrow failure, in which the bone marrow produces too few blood cells of all types (red blood cells, white blood cells and platelets).
“Our bodies have to use stem cells wisely, ramp them up to make more immune cells when they’re needed, but turn off that process when the infection is over, so that we keep a good reserve of stem cells,” said Dr. King, who also is a co-director of Baylor’s Medical Scientist Training Program.
Typically, people are born with 50,000 to 100,000 stem cells in the bone marrow, each producing a portion of about 10 billion blood cells per day. The stem cells that form blood and immune cells are known as hematopoietic stem cells. These stem cells also have the remarkable property of self-renewal, which keeps the body’s blood production system going for an entire lifetime.
As people age, some stem cells acquire mutations. Sometimes a mutation gives a competitive advantage to a stem cell, such as promoting survival or a rapid increase in numbers. The stem cell self-renews, or reproduces genetically identical copies of itself, including the mutation. The stem cell and its clones start to produce proportionally more blood than other stem cells.
About 20 percent of people who are 70 years old have from 4 to 50 percent or more of their blood made from one single mutant stem cell and its clones.
“Those people are 11 times more likely to get leukemia than people without clonal hematopoiesis. What’s even more interesting is that these people are 40 to 50 percent more likely to die from all causes at any given age,” Dr. King said.
Studies have shown that people with clonal hematopoiesis are nearly twice as likely as people without it to die from cardiovascular disease, the leading cause of death in the world.
“Some of the genes commonly associated with clonal hematopoiesis are genes that control inflammation. That explains why you might have more heart disease and stroke, because inflammation causes those diseases,” she said.
Dr. King’s research on the mechanisms by which inflammation affects blood production by stem cells has far-reaching significance. Findings may help develop strategies to protect and enhance bone marrow function for patients with bone marrow failure, cancer, stem cell transplant, chronic inflammatory conditions, and age-associated impaired immunity.
In 2020, the board implications of Dr. King's research led her to win a highly competitive Emerging Investigator Award of $4.2 million over seven years from the National Heart, Lung and Blood Institute (NHLBI) at the National Institutes of Health. This award promotes scientific productivity and innovation by providing long-term support and increased flexibility to investigators whose outstanding record demonstrates their ability to make major contributions to heart, lung, blood and sleep research.
Dr. King previously received national recognition for her research advances in 2019, when she received a Presidential Early Career Award for Scientists and Engineers (PECASE). Established in 1996 to help maintain the leadership position of the United States in science, the PECASE awards are the highest honor given by the U.S. government to outstanding scientists and engineers who show exceptional potential for leadership at the frontiers of scientific knowledge.
Part of Dr. King’s research found another Goldilocks effect related to inflammation and antibiotics.
“Sometimes we have patients who are on antibiotics for a long time, and they get low blood counts. It was never really understood why,” Dr. King said.
“It turns out that you don’t want too much of those inflammatory signals to exhaust your bone marrow, but, on the other hand, you need a little bit. If you have no inflammatory signaling, then you don’t have the normal pressure for stem cells to divide and make new blood cells to keep your body replenished with its normal blood counts,” she said.
Research in Dr. King’s lab demonstrated that the bacteria that normally reside in the gut signal to the bone marrow to help maintain normal blood counts. Antibiotics that eliminate the normal good bacteria in the intestine disrupt the balance.
“We have some clues about metabolites, or small inflammatory molecules that are products of bacteria. The metabolites are absorbed through the intestinal wall and travel through the bloodstream to the bone marrow,” she said.
When the researchers treat mice with broad-spectrum antibiotics, the signal to maintain normal blood production goes away and blood counts drop. But if they feed the metabolites to the mice, normal blood production and blood counts return. A clinical study is underway to determine whether the effect in mice also occurs in people who are on antibiotics.
“That’s a promising line of investigation for our patients. Maybe they’d be able to take a small supplement in their diet while they’re on antibiotics to help protect their blood production and blood counts.”
In another project, Dr. King’s team recently published a paper in the journal Cell Stem Cell related to whether infection contributes to clonal hematopoiesis.
The team’s studies both in mice and with mathematical modeling demonstrated that infection expands stem cells with a common mutation in a gene called Dnmt3a. Although having long-term infection and inflammation could exhaust normal stem cells, the Dnmt3a mutant stem cells resist exhaustion and gain an advantage.
“It’s the first time that anybody has been able to show that an environmental factor – infection – can actually promote the selection advantage and the expansion of these mutant stem cells and thereby contribute to clonal hematopoiesis. It’s a concrete example of how an infection can feed into an evolution of your blood system that predisposes you to cancer and increases your risk of heart disease and stroke,” Dr. King said.
As for future directions? Dr. King and her team are looking further at epigenetics – in which environmental factors change the way DNA works without changing the DNA itself.
“There are some exciting new discoveries in immunology which suggest that stem cells have memory. They respond faster and more efficiently to some pathogens when they see them again. When stem cells come in contact with an infection, something about them is permanently changed and gets passed down to the immune system,” she said.
“We’re contributing to understanding how that works. It has the potential to change outcomes from bone marrow transplants and maybe, even more broadly, how we do vaccinations. It’s a whole new frontier in immunology.”
Discoveries about connections between inflammation and production of blood cells promise greater understanding of a wide range of disease issues and potential improvements in health.