

Texas Children’s Hospital is spearheading an international effort, funded by the National Institutes of Health (NIH) R13 Grant, to identify international priorities for pediatric ECMO and related technologies over the next five to seven years.
The first Pediatric Paracorporeal and Extracorporeal Therapy Summit in October 2022 brought together faculty experts in technologies that support the lungs, kidneys, heart and liver or remove harmful substances from the blood. To improve patient care and outcomes, they are tackling issues in six domains:
By the end of the second summit, planned for 2023, participants in each domain expect to develop frameworks and guidance that may influence areas of research, development and government funding.
Principal Investigators (PIs) on the NIH grant and Meeting Chairs are:
When 3-year-old Kenley Spahn asked for ice cream, it was a welcome sign that she was on the way to recovery from a life-threatening respiratory illness.

The illness had begun with a bad cough and rapid breathing. A visit to an urgent care center resulted in a week on oxygen in a hospital’s pediatric intensive care unit. When her condition continued to decline, her mother, Jess Spahn, insisted on a transfer to Texas Children’s Hospital.
From the moment Texas Children’s Kangaroo Crew team arrived to transport Kenley, the team’s attention and care astounded and reassured her parents.
“When we walked into the ICU room at Texas Children’s, there were no less than 20 people in that room,” her father, Scott Spahn, remembers. “What the entire medical team did was absolutely first class. They gave our daughter back to us.”
To help Kenley breathe, the medical team put her on a ventilator, then, several days later, switched to an oscillating ventilator. When her lung capacity continued to decline, extracorporeal membrane oxygenation (ECMO) was the next step.
ECMO routes blood in a circuit that bypasses the lungs, allowing them to heal. Blood from the body goes through the heart, then through a small tube to the ECMO, instead of the lungs. The blood receives oxygen and then goes back through another small tube to the heart, where it is pumped to the rest of the body.
Ranked first in the country for pulmonology among children’s hospitals for 2023-2024 by U.S. News & World Report, Texas Children’s Hospital Pulmonary Medicine Service provides care for a wide range of complex and chronic respiratory disorders. It also has one of the largest pediatric lung transplant programs in the country.
Texas Children’s Heart Center ranks No. 1 in cardiology and heart surgery for the seventh year in a row. The Heart Center pioneered many of the now-standard procedures and therapies related to the diagnosis and treatment of children with cardiac problems.
Texas Children’s has one of the busiest and most successful ECMO programs in the world. In 2022, the ECMO team cared for 70 patients for a total of 82 ECMO runs, compared to a median of eight cases a year for North American ECMO centers. Outcomes at Texas Children’s are better than international averages.
The Texas Children’s ECMO center has been designated a Center of Excellence at the Platinum level by the Extracorporeal Life Support Organization (ELSO), an international group dedicated to advancing quality, education and research in ECMO worldwide. ELSO has maintained a registry of all ECMO patients at member institutions since 1994. The data are available for research and quality improvement initiatives at those institutions. Only 30 of nearly 600 ELSO designated ECMO centers hold Platinum status, the highest level awarded by ELSO.

Texas Children’s has been providing ECMO support to children with life-threatening lung or heart disease for more than three decades, with outstanding outcomes that are at least in part attributable to a willingness to innovate in the approach to patient care. One of the most successful innovations over recent years is in the early rehabilitation of children while on ECMO.
“ECMO had become synonymous with sedation, even paralysis, and long periods of inactivity that results in children becoming weak, physically and mentally deconditioned. But those of us who have been doing it a number of years have questioned that paradigm. If ECMO provides total physiologic support for your heart and/or lungs, why do you continue to need a ventilator? Especially in children, the endotracheal tube that goes down the throat and connects them to the ventilator is an irritant, and you have to sedate the children so that they remain comfortable,” said James Thomas, MD, Professor of Pediatrics, Division of Critical Care Medicine at Baylor College of Medicine and Medical Director of the ECMO Program at Texas Children’s Hospital.
Sedation requirements are considerably lower for ECMO patients without a ventilator than for patients who remain on a ventilator while on ECMO support. If patients are heavily sedated, this limits their ability to move and gain physical strength and rehabilitate as their lungs slowly recover.
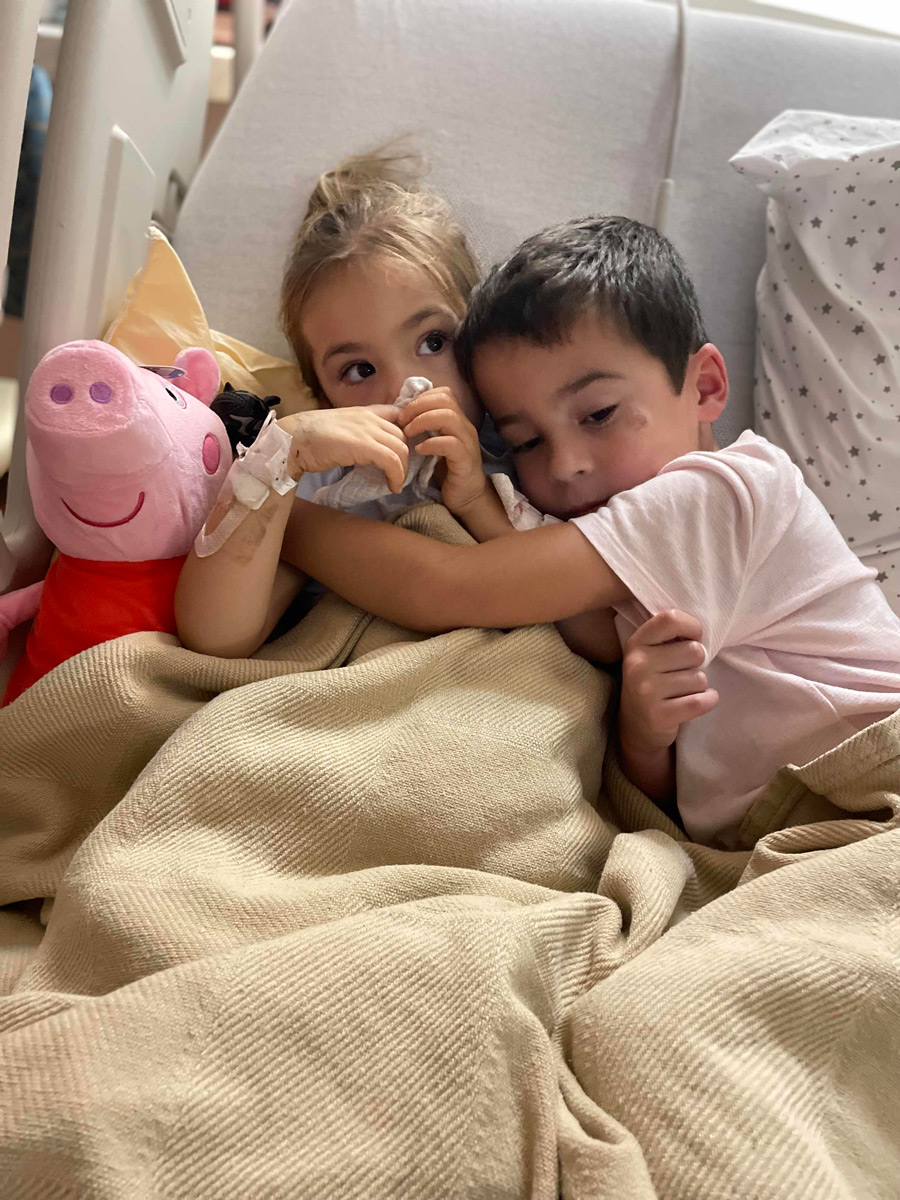
Kenley Spahn had been sedated — and tube-fed — while she was on the ventilator. When Dr. Thomas told her parents that the breathing tube in her throat could be removed, they wondered how she might react.
“They wake her up, and remarkably, she is not at all fazed by these small tubes connected to the ECMO,” Scott said. “They’re in her neck, and they’re strapped to her head. She doesn’t touch them. The only thing she asked for was ice cream.”

The usual ECMO procedure calls for inserting thin tubes, or cannulas, in the patient’s neck or groin. In some cases, however, Texas Children’s uses a technique that differs from the conventional, because the conventional approach does not always provide adequate support to the failing circulation.
In certain types of septic shock, cardiac surgeons open the chest and cannulate the heart directly. When Lara Shekerdemian, MD, MHA, arrived in 2010 as Chief of Critical Care, she brought with her from Australia this treatment for septic shock. Dr. Shekerdemian is now Chair of the Department of Pediatrics at Baylor College of Medicine and Pediatrician-in-Chief at Texas Children’s Hospital.
On occasions, severe bloodstream infection can result in septic shock, with a systemic inflammatory response that leads to cardiovascular collapse.
“With conventional ECMO (with cannulas in the neck or groin), we were not able to flow the blood at high enough rates to save their lives,” Dr. Thomas said. “By placing shorter and wider-bore catheters directly into the heart, we could instead provide an enormous amount of blood flow to support the failing organ systems. We’re probably one of less than half a dozen centers in the U.S. that does that as a matter of routine.”
Some children with right heart failure secondary to severe lung disease are placed on ECMO support while awaiting the lung transplants they require for longer-term survival. Using special cannulas, surgeons can temporarily cannulate the heart directly and close the skin around the cannulas.
“We can now support children waiting for lung transplants with ECMO for many weeks at a time, take the load off their right heart, remove the ventilator, get them up and start to rehabilitate them – even have them out of bed and walking around the intensive care unit if they are old enough. This means that they are in much better physical condition when they receive their new lungs. In turn, this speeds up their recovery after the transplant. We have seen that children who can be awake and rehabilitated while on ECMO do much better after transplant than those who were mechanically ventilated and sedated awaiting their lung transplant,” Dr. Thomas said.
Texas Children’s has developed several additional programs that are rare among ECMO centers, including:
The multidisciplinary team at Texas Children’s made a deep impression on the Spahns, Kenley’s parents. They both expressed special gratitude for the faculty members and fellows from Pediatric Critical Care and Pediatric Surgery.
“The way so many people oversaw our daughter’s care and the way they genuinely cared for her every step of the way was astounding,” Jess said.