

Over the past five decades, great strides have been made in treating many types of pediatric cancers, resulting in an overall cure rate for pediatric cancer that exceeds 80 percent. Despite this progress, brain tumors – the most common solid tumors occurring in children – remain challenging to treat and are the leading cause of death from childhood cancer. One such example is ependymoma, the third most common pediatric brain tumor, for which progress in treatment has stalled.
Ranked No. 6 in the country among children’s hospitals for 2023-2024 by U.S. News & World Report, Texas Children’s Cancer and Hematology Center provides individualized, state-of-the-art medical treatment for patients with childhood cancer and blood disorders. Treating children from 50 states and more than 56 countries over the past 10 years, the center aims to provide the most family-centered, advanced care available.
Scientific advances continue to occur at an increasingly rapid pace and have led to important discoveries about the genetic and molecular aberrations in pediatric cancers. These discoveries have provided physicians and scientists with insights into novel treatment approaches that may benefit children with difficult-to-treat cancers.
There may be hope on the horizon for treating ependymoma using chimeric antigen receptor T-cell (CAR T-cell) therapy, a revolutionary new type of cellular immunotherapy.
Annually, about 200 children in the U.S. are newly diagnosed with ependymoma, a tumor that originates from cells lining the brain and spinal cord. The standard treatment approach to ependymoma includes surgery followed by radiation therapy. Current chemotherapy is usually ineffective.
At diagnosis, ependymomas are treatable. However, more than 50 percent of ependymomas will recur, with diminishing time between subsequent recurrences. There are a limited number of times that additional surgeries and radiation can be safely used, and these treatments can lead to worsening neurological deficits and a reduced quality of life for impacted children. As a result, ependymoma can evolve into a chronic or recurrent disease in which the availability of effective treatment options declines over time. For patients and their families, the fear and anticipation of the next relapse can become overwhelming.
The 10-year survival rate for children with recurrent ependymoma is only about 50 percent.
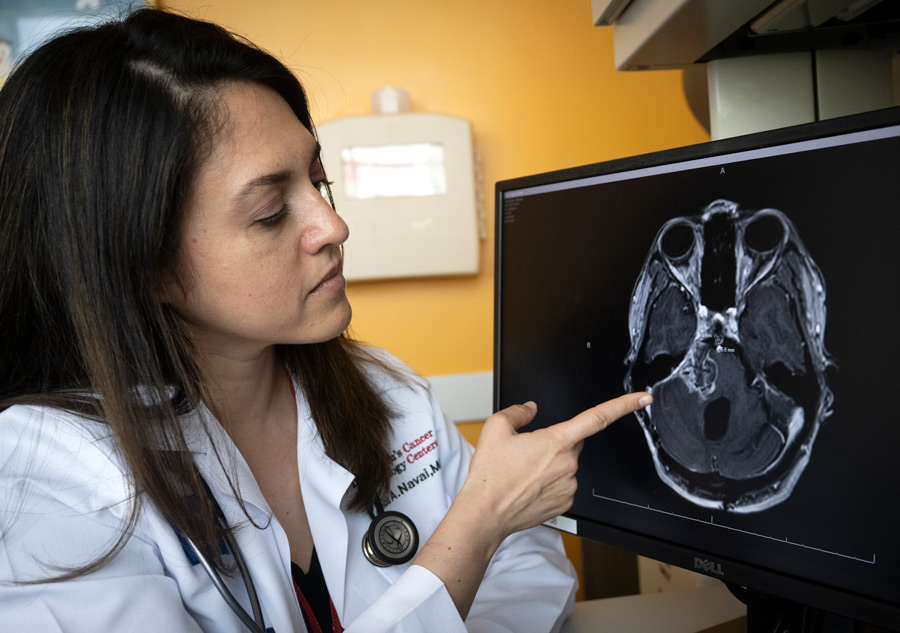
Alongside their colleagues at the Texas Children’s Cancer and Hematology Center (TXCH) and the Center for Cell and Gene Therapy (CAGT), Meenakshi Hegde, MD, Associate Professor, and Shoba Navai, MD, Assistant Professor, both in the Division of Pediatric Hematology/Oncology at Baylor College of Medicine, are optimistic that CAR T-cell therapy may advance the treatment of ependymoma and improve quality of life for affected children.
CAR T-cell therapy leverages the natural ability of the immune system to fight cancer in a targeted way. Genetic engineering of a patient’s T-cells, a type of white blood cell, enables them to express a new protein called a CAR. The CAR redirects these immune cells to recognize and destroy the cancer cells by targeting HER2, a protein expressed on the surface of cancer cells. HER2 is present in about 75 percent of pediatric ependymoma tumors and is correlated with poorer outcomes.
To determine the safety and efficacy of using HER2 CAR T-cell therapy for the treatment of recurrent pediatric ependymoma, Texas Children’s is leading a Phase 1 clinical trial called PBTC-059 through collaboration with the Pediatric Brain Tumor Consortium. This is the first multi-institutional CAR T-cell trial to treat brain tumors in the world.
Twenty-five children will be enrolled in this trial and they will be treated with up to three cycles of HER2 CAR T-cell therapy. Once the treatment is determined to be safe, the clinical trial will be expanded to include a subset of patients who can safely wait a few weeks to undergo surgical removal of their tumor to first receive HER2 CAR T-cell therapy. Following surgery, the research team will assess whether there is evidence of interaction between the tumor cells and CAR T-cells, including an indication of anti-tumor activity.
“This trial provides a unique opportunity to assess precisely what happens to ependymomas at the cellular level following HER2 CAR T-cell therapy, which may provide further insights into why some tumors respond and other tumors do not,” Dr. Navai said.
These findings may also uncover key information about the optimal dosing of HER2 CAR T-cell for future trials.

Established in 1999, the Pediatric Brain Tumor Consortium is funded by the National Cancer Institute. The consortium has 15 member institutions in the U.S. and Canada that are known for their clinical expertise in treating pediatric brain tumors. Most of the study investigators for this trial are based at Texas Children’s, including Dr. Hegde, who serves as the study Chair, and Dr. Navai, who serves as the study’s Co-chair and the site Principal Investigator for Texas Children’s. The study team includes Patricia Baxter, MD, Associate Professor, and Nabil Ahmed, MD, Professor, both in the Division of Pediatric Hematology/Oncology at Baylor.
The HER2 CAR T-cell products are manufactured at the CAGT and shipped to the consortium member sites to be administered locally by medical teams treating patients, enabling patients to receive this novel therapy closer to home. Currently, six sites are enrolling patients:
Several additional sites in the U.S. and Canada are working to enroll patients in the near future.

For patients and clinicians alike, a multi-institutional study offers important benefits.
“Many patients want to participate in clinical trials and gain access to groundbreaking treatments, but for financial and social reasons it is not always possible to travel to a site hundreds or thousands of miles away for extended periods of time. The ability to be treated closer to home opens up more opportunities for patients and leads to higher enrollment, which improves the clinical data and can shorten the trial’s duration, facilitating the widespread availability of the most promising new therapies sooner,” Dr. Hegde said.
“Additionally, this type of knowledge sharing and collaboration between premier pediatric cancer centers can provide new insights or discoveries that may lead to better treatments for ependymoma or other childhood brain tumors,” she said.
For patients with ependymoma, HER2 CAR T-cell therapy could one day be deployed alongside surgery and radiation to enhance the overall effectiveness of these standard treatments while decreasing the frequency of tumor recurrence and associated morbidities.
“Of course, the ultimate goal is complete eradication of ependymoma tumors and the long-term side effects of currently available therapy,” Dr. Hedge said.
The clinical trial officially launched in spring 2022 and is enrolling participants. Patients aged 21 or under with recurring ependymoma are eligible to enroll.