

The team of clinicians and researchers behind the Texas Children’s Hospital and Baylor College of Medicine’s Global TB Program has a singular mission: to advance science to end the global tuberculosis (TB) epidemic.
They hope that the TB GAPS (Tuberculosis Guidance for Adaptable Patient-centered Service) study will be a major contributor toward achieving this goal.
“One of the biggest misconceptions about TB is that it’s a disease of the past. Indeed, TB has existed throughout human history and has killed more people than any other infectious disease over time — but, right now, it continues to impact the lives of people all over the world, across all countries and age groups,” Dr. Anna Mandalakas, MD, PhD, Director of the Global TB Program and Principal Investigator (PI) for the TB GAPS Study, said.
Today, TB remains the leading infectious cause of death globally. Each year, 10.6 million people develop TB. Of this group, 1.3 million people on average die annually. Furthermore, about 1 million children develop TB and 225,000 die on average each year – that’s one child every four seconds.1 Of the children who die from TB, 96% were never diagnosed or had the opportunity to receive treatment.2
Caused by a bacteria called Mycobacterium tuberculosis, TB spreads through the air when infected people cough, sneeze or even sing. The most common symptoms include persistent coughing (sometimes with blood), weight loss, fever, night sweats, chest pain, weakness and fatigue. Without the necessary antibiotics to treat the disease, TB can result in permanent lung damage and can impact other organs in the body, such as the brain, spine and kidneys, eventually causing death.

Even after patients complete treatment, they remain at increased risk for long-term complications, such as cardiac disease, compromised pulmonary function and reduced life expectancy.
Not everyone who is infected with TB develops the disease, though. Approximately 25% of the world’s population have at some time in their lives been infected with TB,3 but they don’t develop the disease or present outward symptoms. People with latent, asymptomatic TB can, however, spread the bacteria to others.
The pediatric population is at an especially heightened risk. Approximately 50% of children less than 12 months of age infected with M tuberculosis develop the disease. Of this group, about 35% will develop severe disease,4 such as TB in the bones and kidneys or meningitis. Children at the highest risk for developing TB are those younger than five years old and those living with human immunodeficiency virus (HIV). These children have either immature or impaired immune function, rendering them incapable of containing the infection. Generally, people with HIV are 16 times more likely to fall ill with TB than people without HIV, and TB is the number-one killer of people living with HIV.1
Compounding the problem is the emergence of drug-resistant TB (DR-TB). This is an issue in which Dr. Debrah Vambe, MD, Baylor and Global TB Program Instructor and Regional TB GAPS Study Manager in Eswatini, has become an expert. According to Dr. Vambe, DR-TB is much harder to treat, because this form of TB must be attacked with alternative drugs for which the bacteria has not developed resistance. In some cases, the bacteria can become resistant to the primary alternative drug and patients develop multi-drug resistance. For the last decade, Dr. Vambe has led the response to DR-TB in Eswatini and served as a resource to partners in surrounding countries, introducing new preventive therapies and evidence-based approaches to treatment.
TB is most prevalent in lower-income countries, particularly those experiencing civil unrest and population displacement. In these areas, a combination of factors often influence poorer outcomes: insufficient diagnostic infrastructure, unaffordability of treatment, the lengthy treatment process, lack of social support for patients undergoing treatment and sub-optimal means of monitoring patients. However, global migration means TB can spread anywhere.
“We know how to treat TB. And yet, our collective inability to eliminate TB is one of the biggest failures of the global health care system,” Dr. Mandalakas said.
According to clinicians on the front lines of fighting TB, the best strategy to defeat the disease is prevention and early detection. But not every health care system has access to accurate tools to prevent, detect and treat TB.
In 2012, Texas Children’s-Baylor launched the Global TB Program, together with Baylor’s Children’s Foundation partners, to promote the health and well-being of people impacted by TB, especially children and those living with HIV. For the last 12 years, the Global TB Program has been central to advancing science to identify the most effective and affordable ways to prevent, detect and treat TB among different populations and settings, while supporting development of clinical laboratory infrastructure, building clinical and research capacity and improving access to health care.
Much of this work has taken place in sub-Saharan African, a compelling region for TB study. Despite comprising just 15% of the global population, Africa is home to 25% of all new TB cases.5 This region also has higher rates of HIV infection, putting the population at greater risk. The underdeveloped health care systems in this area do not typically prioritize preventive care, often lack effective screening and diagnostic tools for rural or under-resourced settings, lack lab capacity to accurately diagnose TB and are not reaching people where they live. As a result, people infected with TB are often found later in the disease’s progression when treatment is more challenging.

In December 2019, the U.S. Centers for Disease Control and Prevention (CDC) requested grant applications to support a five-year study determining the optimal means of preventing, finding and treating TB. For Dr. Mandalakas and her team, they realized what the CDC sought was what the Global TB Program had already been working on for years. Excited by the alignment between the CDC mission and the Global TB Program’s work, the team applied for the study grant in March 2020 and was notified of CDC funding to lead this study in September 2020.
Now known as TB GAPS, this cooperative agreement between the Global TB Program and the CDC extends through 2026, and is implemented at five Baylor Children’s Foundation sites in Eswatini, Lesotho, Malawai, Tanzania and Uganda. The CDC has prioritized these five countries for their high-TB, high-HIV incidence rates. In addition to foundation partners, the TB GAPS study is carried out in collaboration with government partners (including Ministries of Health and national TB and HIV programs in these countries), the CDC Division of Global HIV and TB, the London School of Hygiene and Tropical Medicine and the University of Ottawa in Canada.
The study depends on local experts like Dr. Vambe, with deep regional experience and well-cultivated relationships, to meet with partners and visit clinic sites to coordinate activities and monitor progress, and lead trainings on protocols, sample collection, documentation, diagnosis and treatment.
Together, all these partnering groups are generating substantial evidence to uncover accurate, feasible and sustainable screening and diagnostic strategies, prevent the spread of TB, evaluate the cost-effectiveness of treatment options, examine behavioral drivers behind adherence to a treatment regimen and, ultimately, help to improve treatment and long-term outcomes for those who are diagnosed with TB.
“We are focused on improving TB screening and diagnostics in the world’s most vulnerable children, and hope to ensure that every child combatting TB has a chance to receive life-saving treatment,” Dr. Mandalakas said.
At Baylor Children’s Foundation clinics in these five countries, clinicians screen every patient who shows up for routine HIV care. As of mid-spring 2024, nearly 1,500 patients ranging from infants to 20 years old have been enrolled in the TB GAPS study.
Many exciting developments around screening and diagnostics are underway.
Historically, clinicians have asked patients suspected of having TB four screening questions that relate to cough, fever, weight loss and direct contact with someone known to have TB. Now, consensus is forming among clinicians that these questions lack sufficient accuracy in identifying patients with TB.
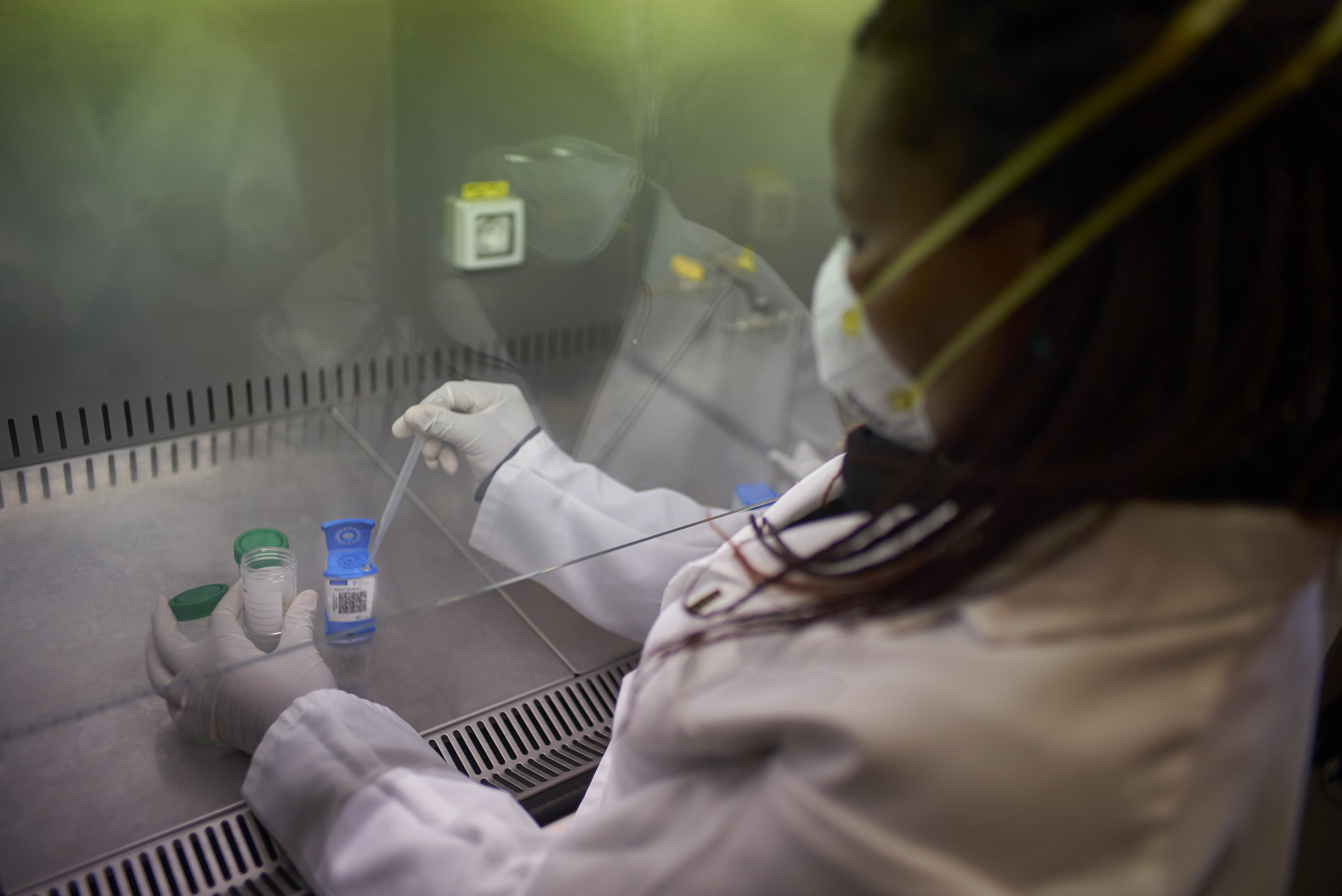
Furthermore, if screening indicates that a patient may have TB, traditional practice has been to run more tests in the form of a chest X-ray and other laboratory tests including analysis of sputum or gastric aspirates. However, children may not have access to these tests or may not be able to produce specimens needed for diagnosis. The TB GAPS team is evaluating other diagnostic methods that are equally accurate yet minimally invasive and simpler, such as finger stick blood samples, stool and urine samples, mouth swabs and face masks to catch respiratory specimens.
Artificial intelligence (AI) also holds much promise in improved detection of TB. Although TB GAPS sites rely on pediatric radiologists to read children’s chest X-rays, computer-aided detection (CAD) can serve as an enhancement of human expertise. CAD is the application of standardized, easily reproduceable diagnostic algorithms to X-ray images to efficiently generate a score indicating the likelihood of the presence of TB. In countries with shortages of pediatric radiologists, CAD can mitigate limited human resources. In less accessible areas, CAD can be added to mobile units to diagnose patients in the field, in real time.
To foster connections and share knowledge and practices about TB prevention, diagnosis and treatment with other researchers, clinicians and public health professionals in the region, the TB GAPS team has leveraged ECHO HUB, a virtual learning platform that aims to sustain the impact of the study long after its completion. ECHO HUB now has more than 150 participants in 12 countries.
Additionally, the TB GAPS Study is helping to develop research capacity in partner countries through U.S. National Institutes of Health (NIH) International Center-sponsored training grants that support independent researchers of TB.
The TB GAPS study is moving forward with great partner collaboration and multi-stakeholder participation.
So far, research findings from TB GAPS and other Global TB Program projects have already informed policy and practice changes at the clinical, national and global levels, and the Global TB Program team is regularly engaged in updating guidelines in care and treatment of TB among children at the country level and with the World Health Organization (WHO). These changes have made an elevated, globally recognized standard of care accessible to more people, promoting health and saving lives.
An example of a major success story is the treatment of drug-resistant TB (DR-TB).
“DR-TB used to take two to three years to treat. Now, we’ve introduced an effective combination of fewer drugs that is less costly and shortens treatment, which increases the likelihood of compliance with the full course of treatment. As of 2022, we can treat DR-TB in just six months, which is comparable to treating regular TB cases,” Dr. Vambe said.
The study is also revealing some surprises that will contradict previous assumptions about TB in the medical community.
“We have found some results that we did not anticipate. Information from this project will fill huge gaps in the evidence and provide new evidence that will inform our mission to eliminate TB globally going forward,” Dr. Mandalakas said.