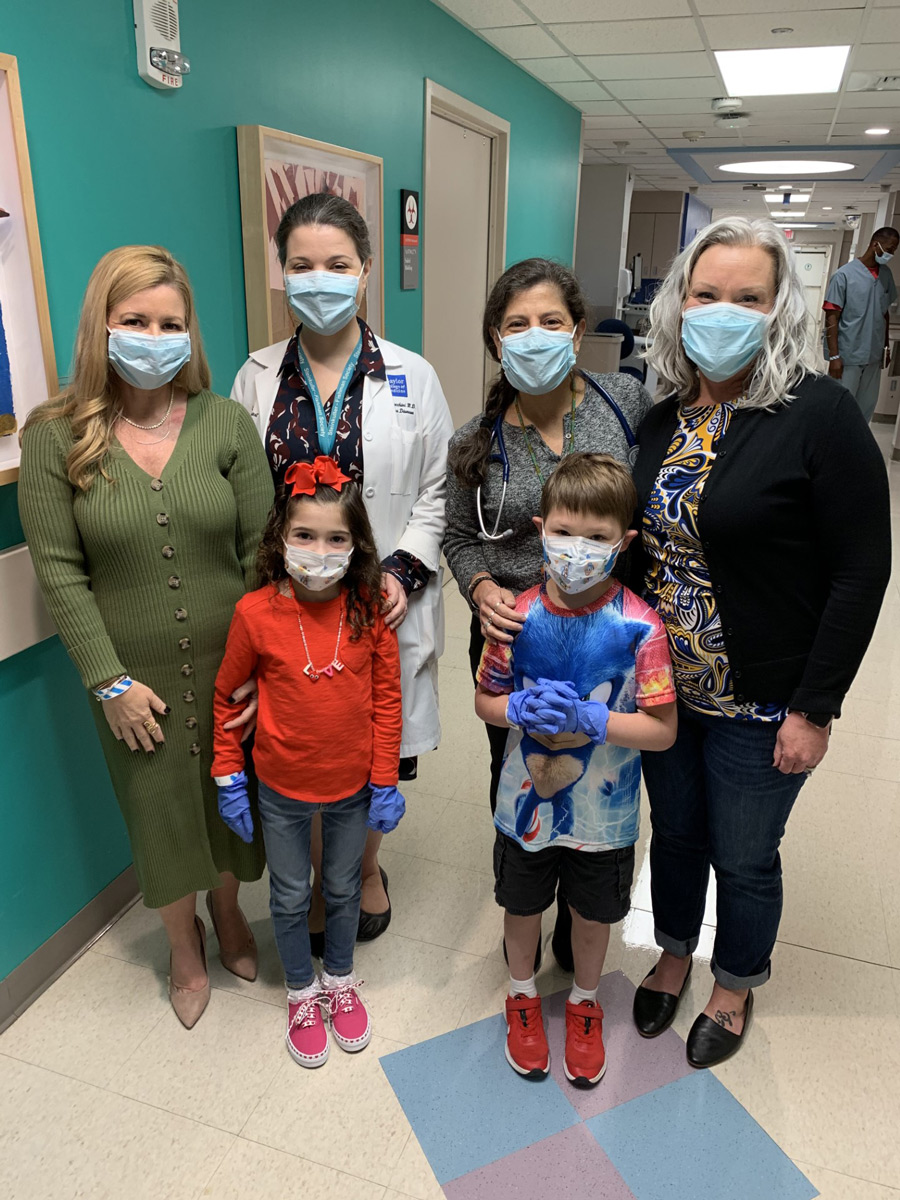
Before she was 5 years old, Juliana Graves, 9, had 20 stays at Texas Children’s Hospital because of infectious diseases. The reason? Her immune system was suppressed to prevent rejection of the life-saving heart transplant she received when she was only 17 days old, the youngest heart transplant patient yet at Texas Children’s.

After an organ transplant, immunosuppression is a double-edged sword. Improved therapies have greater ability to prevent the immune system from attacking or rejecting the transplanted organ. At the same time, reducing activity of the immune system also reduces protection against infection. Infection has become one of the most frequent — and serious — dangers for solid organ transplant patients.
Because of the dangers of infection, the Transplant Infectious Disease (ID) Service is an integral part of the Transplant Services team at Texas Children’s Hospital. Texas Children’s is unique in that it has a physician service line dedicated to pediatric transplant ID.
Texas Children’s leads the nation in pediatric solid organ transplants. The team has transplanted 2,100 organs since 1984 — including heart, kidney, liver and lung. In 2022, the team successfully performed 99 transplants, outpacing all other children’s hospitals by more than 20 surgeries. The comprehensive and multidisciplinary transplant team cares for patients — from infants to young adults — with the most complicated conditions.
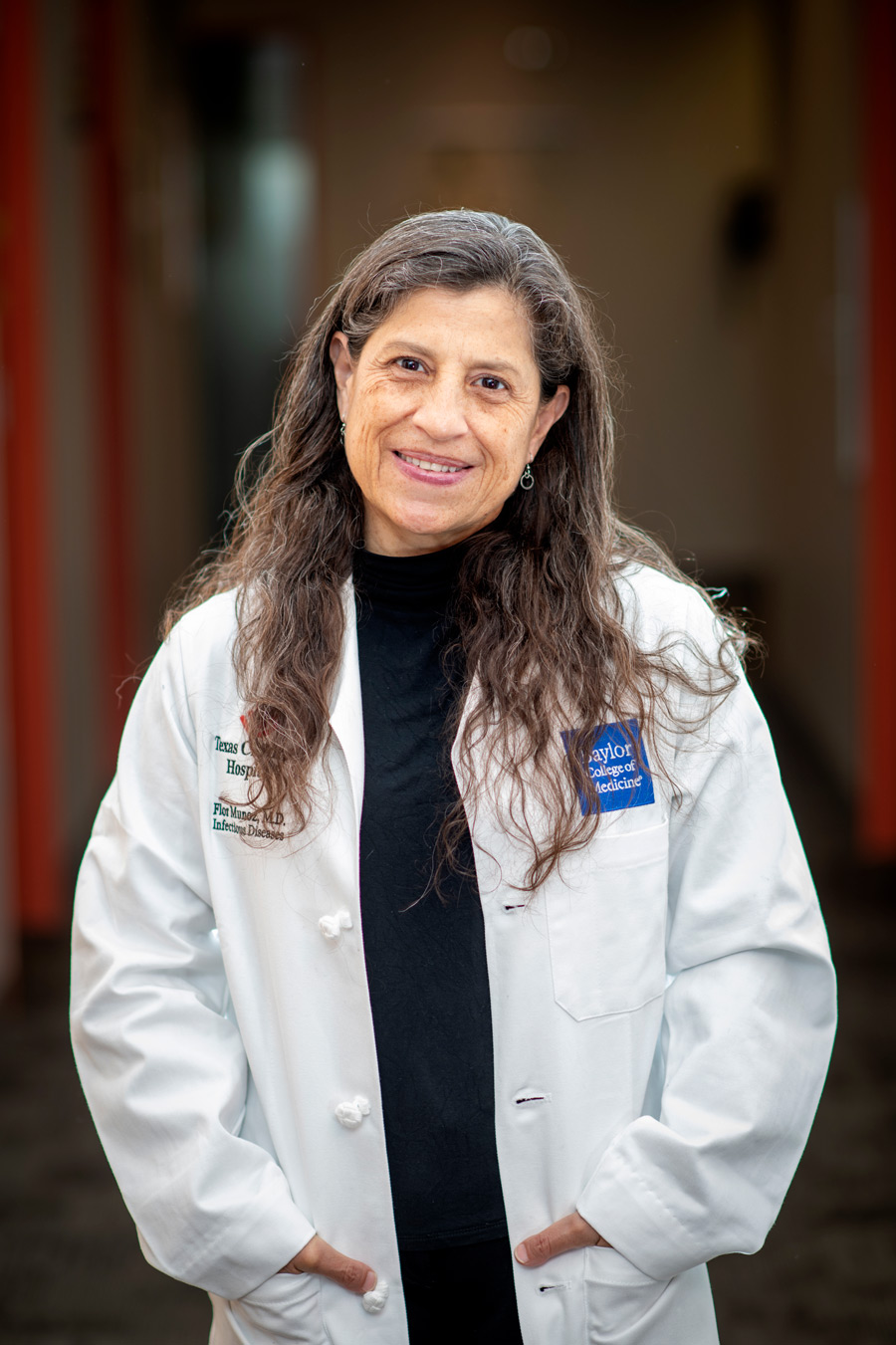
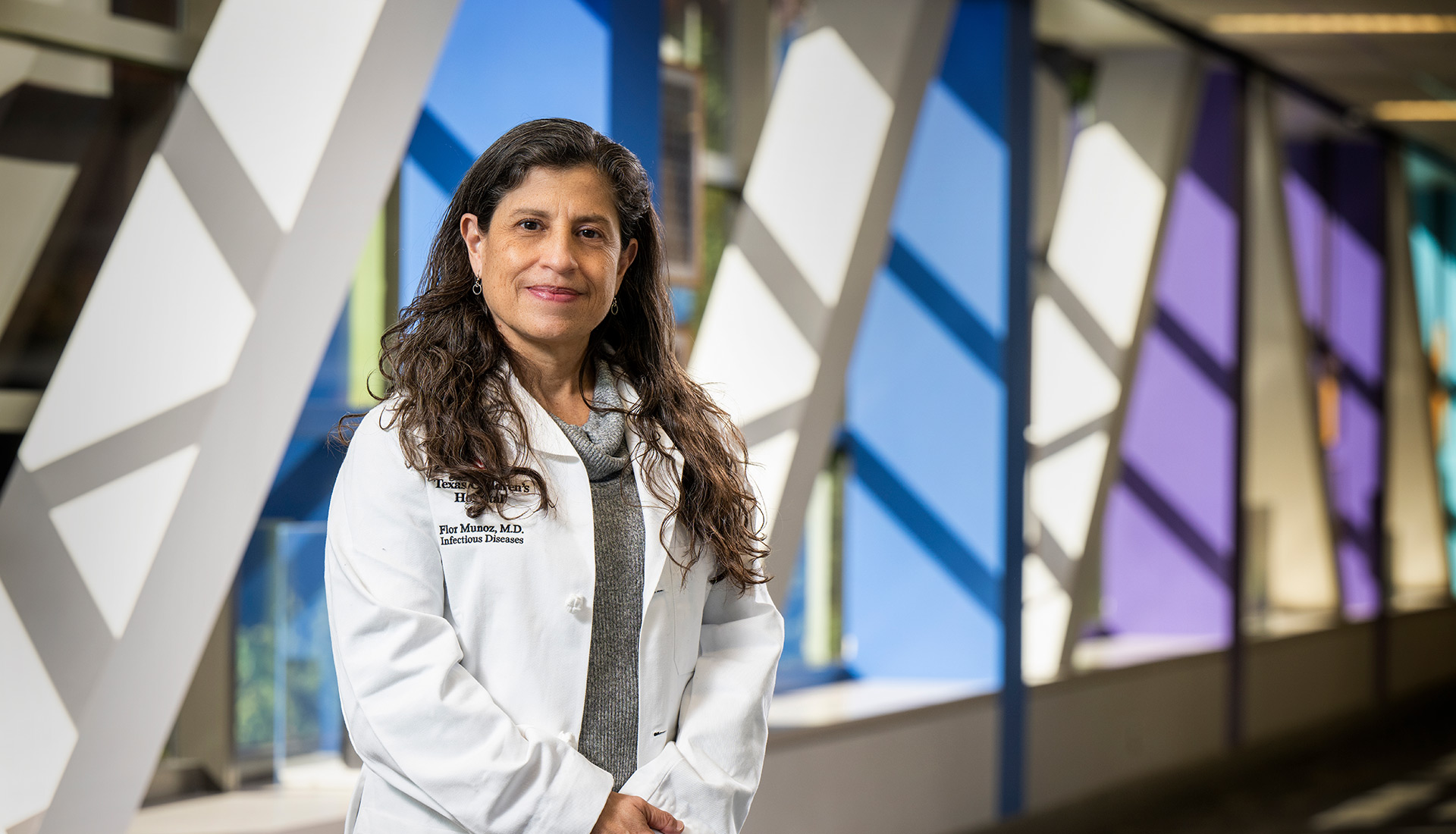
“We know these patients from day one when they are evaluated for transplant candidacy, and we follow them throughout the transplant process,” said Flor Muñoz, MD, Director of Transplant ID at Texas Children's and Associate Professor of Pediatrics-ID at Baylor College of Medicine. “This longitudinal care approach allows for better care, better outcomes, and establishing a close relationship with the medical team and with the patients and their families.”
Started by Dr. Muñoz in 2011, the Transplant ID program has grown to five faculty physicians and one advanced care nurse practitioner. The transplant ID team sees patients from pre-transplant evaluation through and after transplantation, following them in the clinic or in the hospital for any infectious disease-related issues, ensuring that they are up to date with their immunizations and taking preventive treatments to reduce the risk of infections.
“We become the patient’s ID doctors for as long as they need us,” Dr. Muñoz said. “Team members are available 24/7 for infectious disease-related questions about organ donors and recipients and to care for our patients when they are in the hospital or at home.”
Transplant ID team members meet twice a week to discuss patients. They actively participate in multidisciplinary rounds and meetings with Transplant Services organ teams every week.

Infection is an important cause of hospitalization and death in transplant patients, and this is because they have a weakened immune system making them particularly vulnerable to serious bacterial, viral, fungal, molds and yeast infections. A child with a normal immune system usually recovers well from common viruses, such as Epstein-Barr virus (EBV), the cause of mononucleosis, and cytomegalovirus (CMV), which usually causes a self-limited fever illness in healthy children. For someone who has recently had a transplant, however, these viruses can make them extremely sick.
Similarly, chicken pox, which is usually mild in children, can be deadly in someone with a suppressed immune system. Suspected chicken pox sent Reid Burrell, 9, to the emergency room in 2018. Reid takes immunosuppressants because he had a life-saving liver transplant when he was 10½ months old.
“He was admitted for three days for testing and treatment out of extreme caution until his labs could rule out chicken pox,” said Reid’s mother, Heather Burrell. After it was determined that his illness was not life-threatening, she said, “we got to go home and live our life.”
In 2020, Heather got shingles, which is caused by the same virus as chicken pox. After consulting with Dr. Muñoz, Heather stayed with her parents until she recovered to avoid the risk of giving Reid chicken pox.
“We can take precautions in the daily lives of children who have had transplants to decrease the impact of those risks on their quality of life. We talk to families about the importance of hand-washing, avoiding sick contacts, and regular dental care, because having healthy teeth decreases the risk of infection,” said Claire Bocchini, MD, Assistant Professor of Pediatrics-Infectious Diseases and Pediatric Transplant ID Track Director for the Pediatric ID Fellowship program at Baylor.
“Vaccines are a wonderful way to train the immune system to protect our patients. If we can get them vaccinated before transplant, that helps their body maintain the protection after transplant. We also talk about the importance of vaccines for family members because we want to minimize the risk of vaccine-preventable diseases coming into the home,” Dr. Bocchini said.
Juliana’s mother, Riki Graves, MHA, has worked with Dr. Bocchini to become a vaccine advocate, testifying at the state legislature on the importance of vaccine policy in Texas. Riki recently was appointed to the Organ Procurement and Transplantation Network’s Disease Transmission Advisory Committee as part of the United Network for Organ Sharing.
The Transplant ID team works closely with others in diagnosis and treatment.
“We collaborate with our microbiology laboratory, and with experts at other institutions if necessary, to use the most appropriate and specific diagnostic tests and treatments for our patients,” Dr. Muñoz said. “Because transplant patients may need to receive many treatments with antibiotics, bacteria may develop resistance. In situations where we are running out of options for treatment, we may even consider a research trial or compassionate use access to medications that we can use to treat a serious infection.”
In addition to clinical care, the team participates in quality improvement, research and education. ID fellows can choose the Pediatric Transplant ID Track during their fellowship. Also, team members mentor students and colleagues from other specialties, such as critical care, cardiology or hepatology, who are interested in the field.
About eight years ago, Dr. Muñoz and former Baylor faculty member Laila Woc-Colburn, MD, (adult ID specialist) started a Transplant ID Collaborative group featuring monthly meetings within the Texas Medical Center. The membership and participation in this meeting have significantly opened up, particularly since virtual meetings began during the COVID-19 pandemic. Now, 35 to 50 specialists and trainees from as far away as Madrid, Spain, and representing both pediatric and adult expertise in transplantation, join the monthly educational meetings.
“At Texas Children’s, we do a lot of transplants, and we have excellent transplant patient outcomes and graft survival,” Dr. Muñoz said. “What makes us stand out is that we have teams exclusively dedicated to our transplant patients. In addition to the specialists performing the transplants, nurses, pharmacists, physical therapists, psychologists, respiratory therapists, nutritionists, radiologists, and many other subspecialty experts and consultants constitute the Transplant Services team. It is a highly specialized and cohesive team that allows us to manage our patients and take care of their needs using a multidisciplinary approach.”
Dr. Muñoz credits John Goss, MD, and the medical surgical leaders for solid organ transplants, for the development of the well-integrated Transplant Services. Dr. Goss is Medical Director of Transplant Services at Texas Children’s and Professor of Surgery and Chief of the Division of Abdominal Transplantation at Baylor College of Medicine. She also credits support from the Department of Pediatrics and the ID Division leadership for the success of the overall organ transplant program and the Transplant ID Service.
“One thing I really love about the transplant program is that we work closely with the transplant teams over the years, so some of the patients that I saw today are the same patients I took care of in 2013 or 2014,” Dr. Bocchini said. “It's just amazing to be able to see why we do this, to see these kids grow up and get to do all the things that kids who don't need a transplant get to do.”