Interventional pediatric cardiology continues to be a rapidly advancing field, with an increasing number of heart conditions treated through minimally invasive, catheter-based interventions. Interventional Cardiology at Texas Children’s Hospital is the largest program of its kind in the region, performing over 1,400 cardiac catheterization procedures in 2019. The Charles E. Mullins Cardiac Catheterization Laboratories were included in the Lester and Sue Smith Legacy Tower expansion and the Heart Center now operates four catheterization labs and an adjacent intra-catheterization MRI suite. This state-of the-art environment allows greater access to care for patients needing cardiac interventional and imaging expertise. Our catheterization labs and advanced MRI diagnostics can be used in a single episode of care to determine how to best intervene in a patient’s condition, but to also immediately determine the effectiveness of the intervention. In 2019, we performed approximately 30 procedures utilizing MRI and cardiac catheterization procedures in the same setting.
Our expansion into Legacy Tower allowed for the introduction of a new generation of catheterization lab systems. The use of this technology directly reduces radiation exposure for our patients without a compromise in imaging. The application of best practices and the innovation of techniques has positioned the Interventional Cardiology service at the forefront of cardiac medicine. We now have seven full time interventional cardiologists, three of whom are certified in Adult Congenital Heart Disease as well. Our faculty is actively involved with research that allows for new treatment strategies and device usage that will lead to enhanced patient outcomes. Much of the research work is multi-center and multi-year clinical trials. Our recent works include:
- Clinical trial of closure of patent ductus arteriosus using the new Amplatzer® Duct Occluder II Additional Sizes (ADO-II AS/Piccolo Occluder) and development of a comprehensive program for treating small children with PDAs
- Clinical trial of closure of atrial septal defects with the new ASSURED trial using the Gore Cardioform ASD device (the highest enrolling site in the country, device now approved by the US FDA)
- Clinical trial of transcatheter implantation of the new Medtronic Harmony® valve in patients with pulmonary insufficiency
- Clinical trial of transcatheter implantation of the new Edwards Alterra® pre-stent system in patients with pulmonary insufficiency
- Post-approval study of transcatheter closure of muscular ventricular septal defects using the Amplatzer® Muscular Septal Defect Occluder (the highest enrolling site in the country)
- Lead national site for the Congenital Cardiovascular Interventional Study Consortium (CCISC) Coronary Artery Fistula Registry
In addition to participating in important clinical trials, our Interventional Cardiology team, in conjunction with the cardiac surgical team, has developed a comprehensive Pulmonary Vein Stenosis program, one of the largest in the country. With a focus on cutting-edge technology, this comprehensive program has improved the outlook for many patients with pulmonary vein stenosis.
We have also developed comprehensive collaborative programs within our hospital focusing on pulmonary hypertension and children with bronchopulmonary dysplasia (BPD).
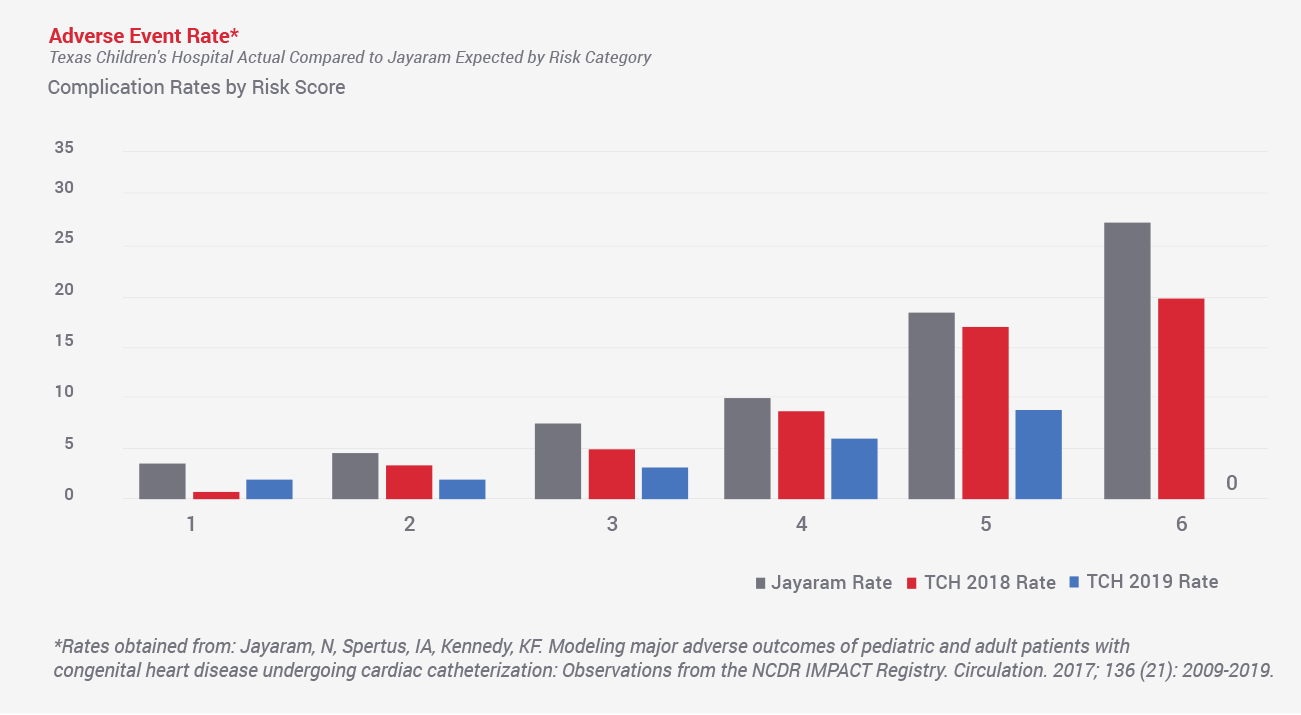
The Interventional Cardiology team also has a clear focus on outcomes and quality. The team’s expertise spans from common disease management to less common, highly complex patient conditions. Implementation of pre- and post-procedure risk assessment has become a standard for every patient we care for. That assessment, combined with close monitoring of our complication data, allows our team to compare our outcomes to national benchmarks. Our adverse event rate has been consistently less than the national benchmark in all risk categories and these rates continue to improve over time.