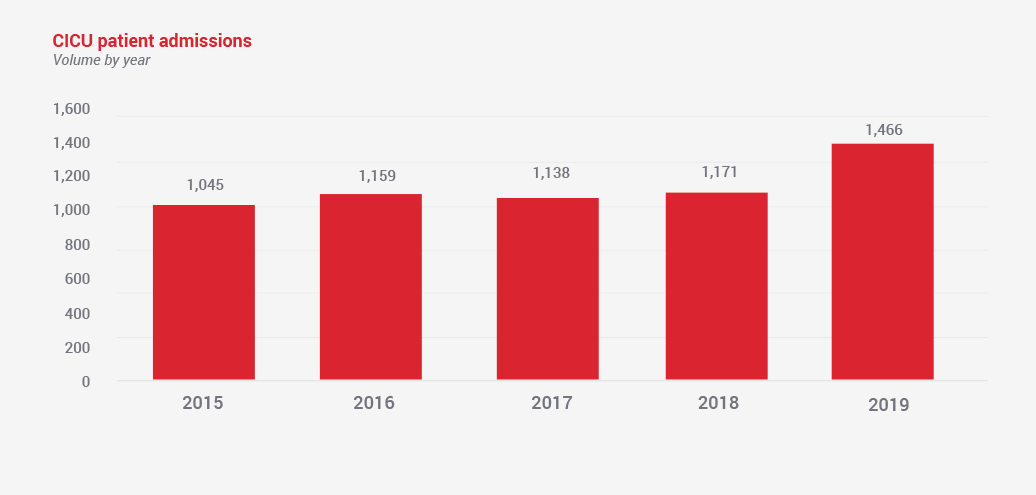
The Cardiac Intensive Care Unit (CICU) at Texas Children’s Hospital strives for continued excellence in the care of infants, children and adults with complex cardiac disease. The patient- and family-focused multidisciplinary care delivery model is supported by some of the best specialists and care providers in the nation, ensuring the highest level of clinical support for some of the sickest children in our region and beyond. The CICU, which houses 54 state-of-the-art CICU rooms, all with dedicated family space, spans three floors, in direct adjacency or vertical proximity with the cardiovascular operating rooms, catheterization laboratories, MRI scanners, interventional radiology suites and all other support services. The CICU is also collocated with the 84-bed Pediatric Intensive Care Unit.
The CICU Team
The CICU is staffed by a highly experienced, multidisciplinary team of physicians, advanced practice providers, nurses, respiratory therapists and pharmacists, as well as a nutrition team, physical therapists and occupational therapists. All members of the team and the patient families are included in multidisciplinary rounding with shared decision-making. We are actively involved in numerous collaborative clinical, quality and research initiatives. Our growing group of dedicated CICU advanced practice providers, together with more than 40 ACGME fellows in cardiology and critical care medicine, provide patient care under the supervision of our 34 cardiac intensivists with subspecialty training in pediatric critical care, cardiology, neonatology and cardiac anesthesia. The Cardiac Critical Care Instructorship program is nationally recognized for innovations and leadership in training the next generation of pediatric cardiac intensivists. Specialized complex care patient teams monitor patient progress, developing plans for interventions and optimizing supportive therapies to achieve the best outcomes in some of the most complex patient populations, such as patients with hypoplastic heart syndrome. A dedicated Heart Center Rapid Response Team is staffed by intensive care attendings, fellows, nurses and respiratory therapists, ensuring timely escalation of care and transport of patients to a higher level of care.
Subspecialty Cardiac Intensive Care
The CICU environment includes 54 patient beds, allowing us to further expand our subspecialty focus for critically ill children with heart disease. We have a 12-bed dedicated Heart Failure Intensive Care Unit, the first of its kind in the nation, which focuses on the treatment of children with heart failure and those requiring intensive care before and after heart transplant including both durable and temporary mechanical circulatory support strategies. In 2019, we offered both pulsatile and continuous durable ventricular assist device support to patients allowing for optimal recover and rehabilitation while awaiting heart transplantation. In addition, we have a neonatal CICU which cares for newborns before and after cardiac surgery. The creation of a neonate-oriented environment with strong focus on their developmental care, while attending to the specific needs of their families, helps optimize the patient’s post-operative growth and development.
Quality and Outcomes
The outcomes and performance of our CICU are closely monitored through participation in national registries including Pediatric Critical Care Consortium (PC4), Extracorporeal Life Support Organization (ELSO), Society of Thoracic Surgery (STS) and Pediatric Interagency Registry for Mechanical Circulatory Support (PediMACS). Our Heart Failure ICU is also an active participant in the Advanced Cardiac Therapies Improving Outcomes Network (ACTION) collaborative focusing on improving outcomes for pediatric heart failure and ventricular assist device patients. Patient safety and quality are monitored by our quality team, with regular reviews of all of our practices and procedures. Internal audit routinely includes benchmarking our performance alongside other high-volume U.S. centers.
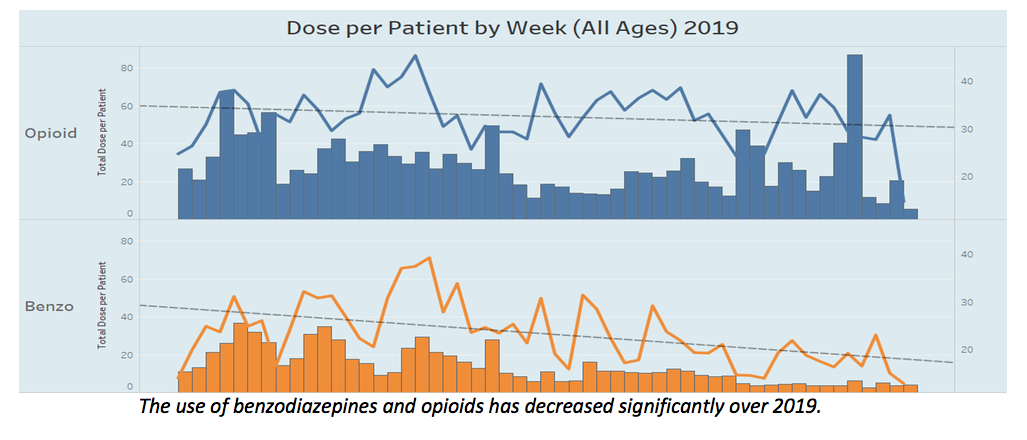
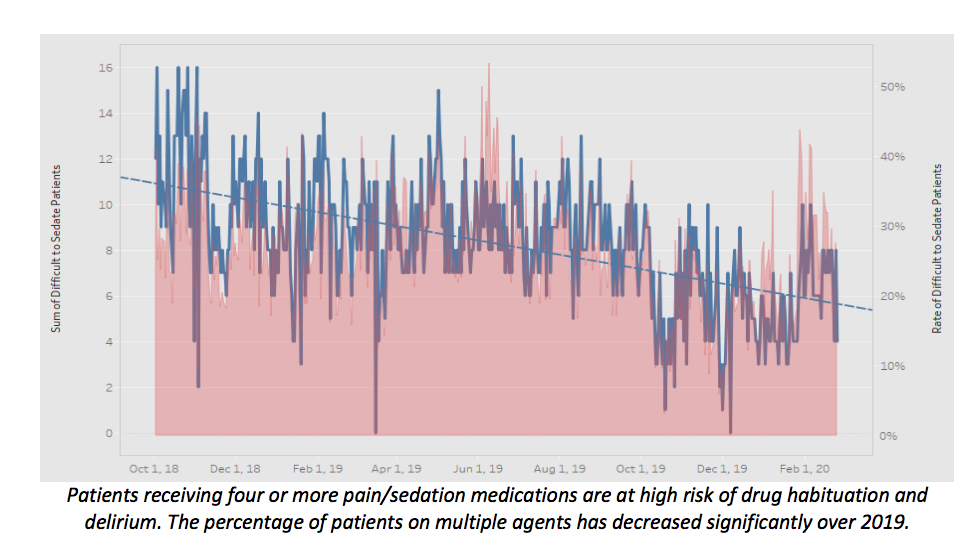
A primary focus in the critical care of post-operative patients is comfort, pain management and safety of medical devices. Emerging clinical and outcomes data has shown that unchecked sedation and pain control practices can lead to prolonged length of ICU stay and can have deleterious neurodevelopmental effects for pediatric patients in the CICU. The team of experts committed to reduction in use of sedative medications utilize various data visualization platforms to help our providers make informed data driven decisions at the point of care. The physicians, providers and pharmacists utilize a number of medication dashboards to ensure that use of sedatives in CICU is focused and dosed, according to standardized protocols. The dashboards organize data for each individual patient and enable clinicians to view exposures and customize strategies in weaning plans. Ongoing evaluation of aggregate data has shown that use of dashboards and review has led to a 30% decreased exposure and 20% reduction in use of multiple sedative agents.
Extracorporeal Cardiopulmonary Resuscitation
Extracorporeal membrane oxygenation (ECMO) is now considered a standard treatment option for infants and children with severe circulatory failure. Extracorporeal cardiopulmonary resuscitation (ECPR) refers to the initiation of lifesaving ECMO in the setting of cardiac arrest. Successful ECPR outcomes require rapid team deployment, quick decision-making and extensive team training to ensure best outcome of this life saving therapy. Texas Children’s CICU has an expert mechanical circulatory support team available 24 hours a day allowing for rapid initiation of the support with an improved call-out and response system, and enhancement of the availability of key personnel around the clock. In 2019, we deployed this advanced treatment in 12 cases.
International Collaborations
Our Critical Care department has established strong links with cardiac teams in several countries within Latin America. Through videoconferences with our colleagues in Mexico City, we have established regular virtual ward rounds and additional communication forums, rounding with the local cardiac surgeons and intensivists in their two main cardiac centers. In 2019, we held more than 70 videoconference ward rounds in the two CICUs in Mexico City, assisting with patient management, sharing clinical protocols, establishing new or innovative therapies including ECMO, and recommending quality improvement initiatives. In addition, together with many Heart Center colleagues, our critical care team has active educational and simulation-based collaborations with several centers in Latin America (Mexico, Chile, Colombia, Argentina and Costa Rica) aimed at developing advanced perioperative cardiac care and to establish and maintain ECMO programs. Numerous CICU faculty members, providers and nurses volunteer and spend clinical time on congenital heart surgery mission deployments, to provide care to children after cardiac surgeries in developing countries.


